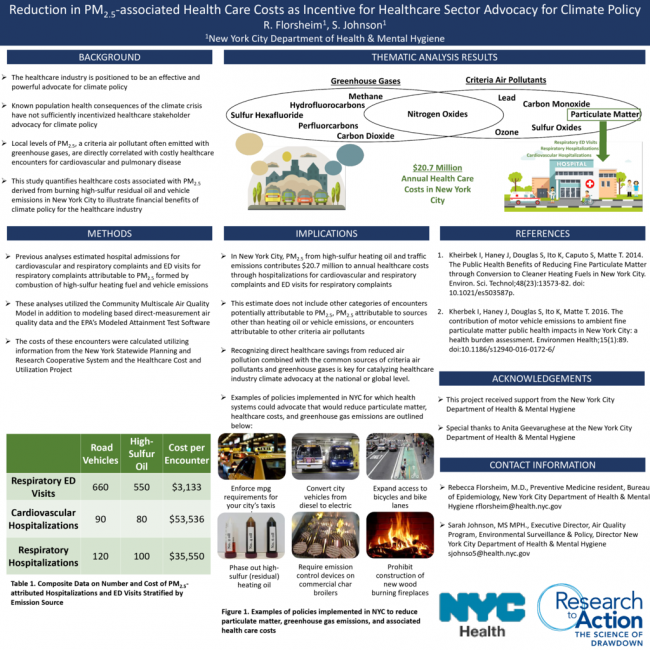
The nature and extent of adverse health outcomes exacerbated by the climate crisis are firmly established. The scientific community has consistently appealed to the healthcare sector to intervene on climate change for the benefit of population health, but also because of the sizeable percentage of greenhouse gas (GHG) emissions attributed to the healthcare system and the significant lobbying power of hospitals and insurers. However, suggested interventions often lack sufficient direction or incentive for healthcare stakeholders to advocate for effective climate policy. Indeed, unrealistic, expensive, or disruptive calls to action such as reconfiguring hospital supply chains or changing clinical protocols to reduce greenhouse gas (GHG) emissions have yielded little progress. Attempts to engage hospitals and insurers in climate action also traditionally highlight the consequences of a warming climate and GHG emissions rather than those of PM2.5, a criteria air pollutant often emitted with GHG, known to be highly correlated with acute asthma exacerbations, respiratory infections, and hospitalizations due to cardiovascular disease. In New York City, PM2.5 produced by burning of high-sulfur heating fuels and traffic emissions alone is estimated to contribute $18.9 million to annual city-wide healthcare costs. Yet, statistics highlighting the financial relationship between the combustion processes that produce GHG and PM2.5 and direct increases in healthcare costs are mostly absent from conversations in healthcare regarding the climate crisis. We assert this relationship is key to aligning the incentives of the scientific and healthcare communities to provide a framework for effective lobbying for climate policy.
Day
Tuesday Poster Session
Related Conference Themes
Built Environment
Electricity Generation
Transportation